International Hepato-Pancreato-Biliary Association
Laparoscopic distal pancreatectomy with possible splenectomy [case 14]
Surgeon's Impressions
Watch the following videos of the surgeons preoperative plans for the case. Compare their findings with your own analysis.
Critical imaging findings:
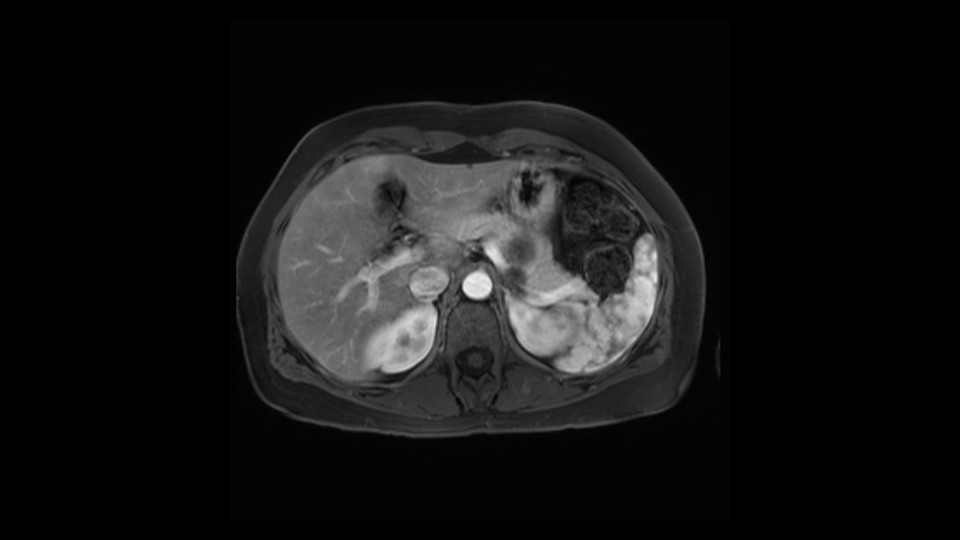
Cystic nature of lesion
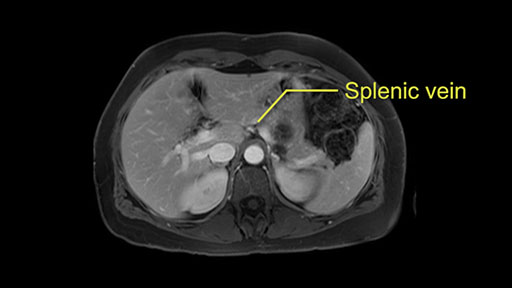
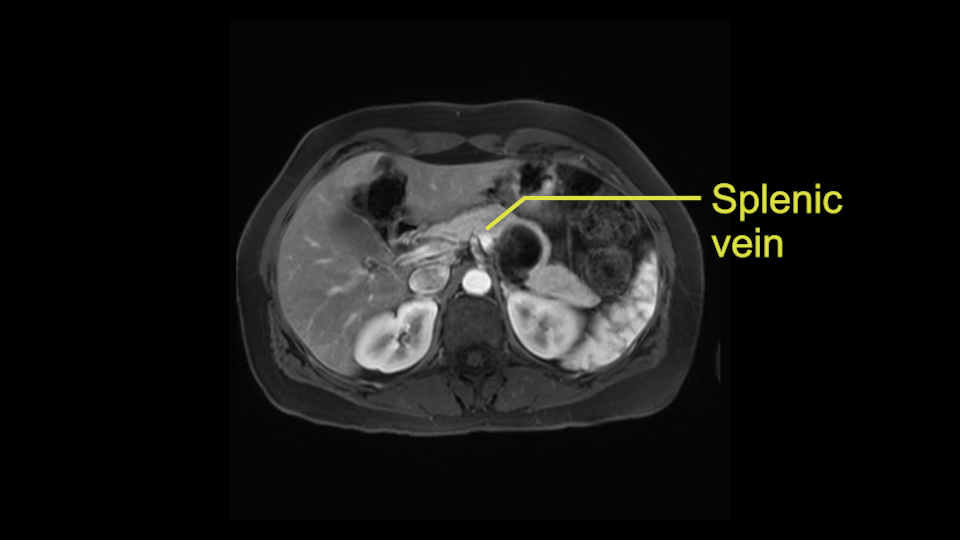
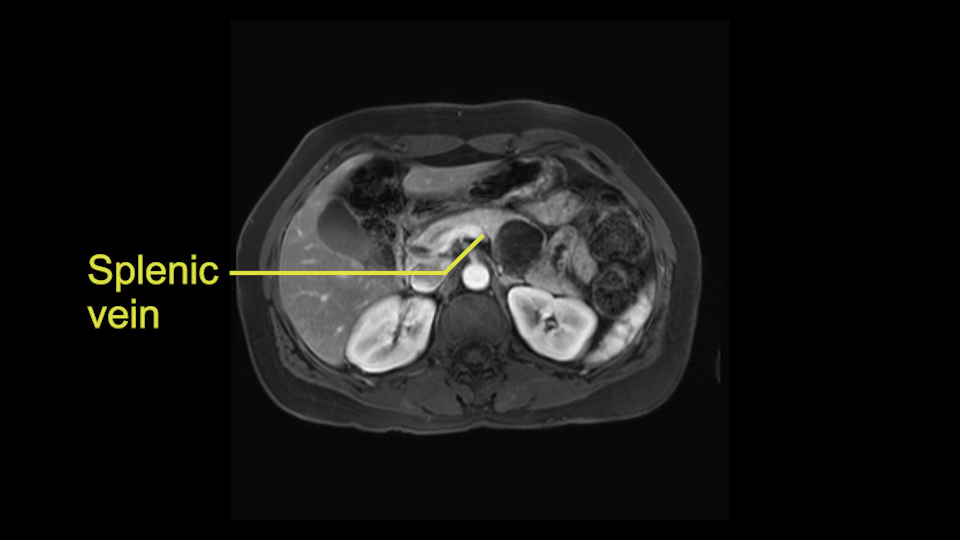
Tumor proximity to splenic vein
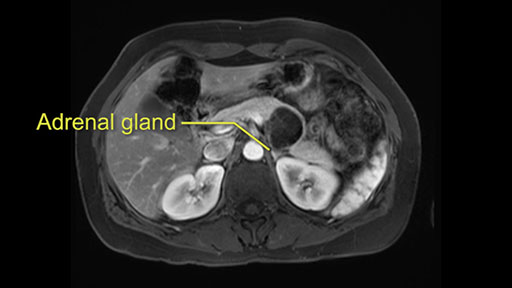
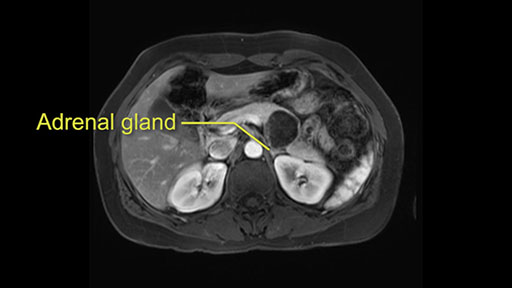
Tumor proximity to left adrenal gland
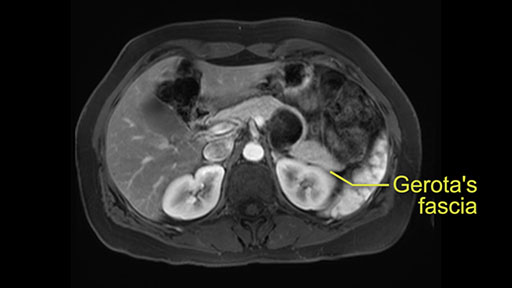
Posterior pancreas margin: Gerota's fascia
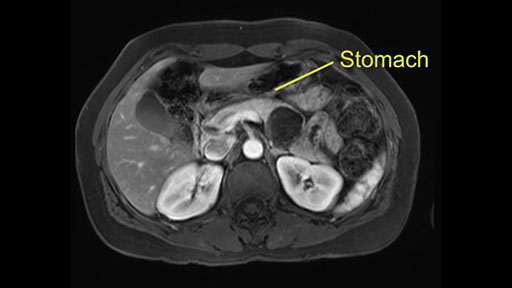
Anterior pancreas margin: posterior wall of stomach
My name is Sean Cleary. I’m an associate professor of surgery at the University of Toronto and a hepatobiliary and pancreatic surgical oncologist at the University Health Network. This patient is a 48-year old woman with a cystic neoplasm in the pancreas and this lesion was found incidentally after an ultrasound was performed to diagnose kidney stones. It was asymptomatic and the patient had no history of pancreatitis. The case was reviewed at a multidisciplinary tumor board round. Due to the risk of malignancy within this lesion, surgical resection was recommended.

For me, the slowing down moments in this operation are: The handling of the tumor itself and mobilization of the pancreas. This is a cystic lesion, the wall can be quite thin and you do not want to risk intraoperative rupture of the cyst as that can cause spread of pre-malignant or even malignant cells.

The second slowing down moment is the decision whether to perform a splenic preservation procedure or include a splenectomy with this procedure. That would require maintaining adequate splenic perfusion and inflow to allow spleen preservation. The decision is both a technical question as well as an oncologic one, and therefore we need to evaluate both of those issues in combination.

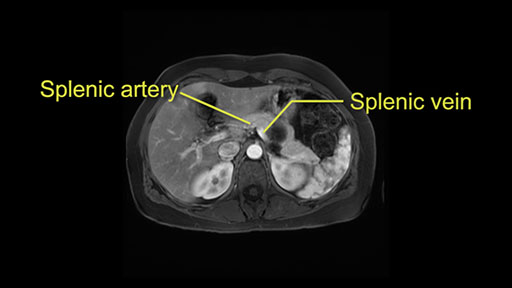
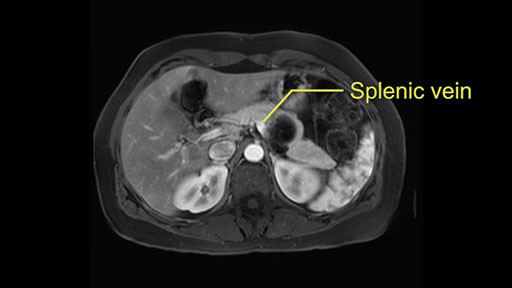
Other slowing down moments with this procedure include dissection of the splenic vein and splenic artery. These are technically challenging moments and important moments where care needs to be taken. Not only to avoid bleeding and injury to the vessels but also to ensure an adequate margin.
Additional slowing down moments are: division of the neck of the pancreas - to ensure that you obtain an adequate margin within the pancreas.

Other slowing down moments include: if you’re going to perform a spleen preserving procedure, dissection of the pancreatic tail at the level of the splenic hilum. This area can be difficult and we’ll need to ensure that we proceed without causing bleeding. Also ensuring that no pancreatic tissue is left behind within the splenic tail because a perfused remnant can be a significant complication.
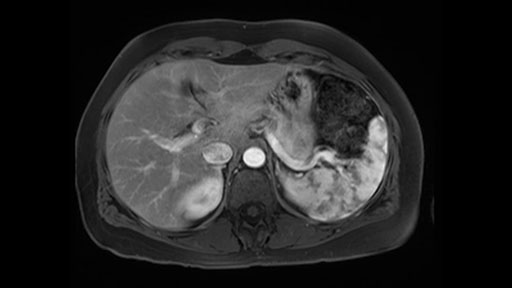
In reviewing this patient’s CT scan, first of all, the lesion is again cystic with a very thin wall. I anticipate that it will be delicate and potentially friable. And therefore the risk of rupture exists and we need to be very careful in how we handle the pancreas and the tumor throughout the procedure.

The lesion itself is quite adjacent to and abuts the splenic vein and therefore we need to anticipate that these two structures will be intimately related and possibly impossible to separate between the two.
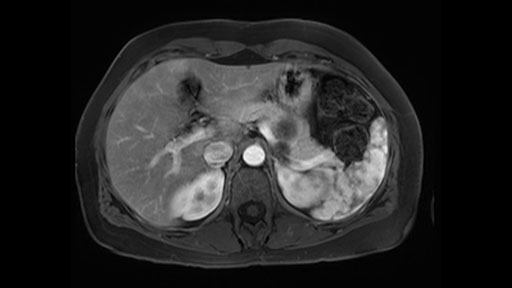
The lesion also is quite posterior. While the plane between the cyst and the left adrenal gland is often preserved, we do have to pay attention here so that we remain in the right plane and maintain our margin here. Occasionally in these cases, en bloc adrenalectomy needs to be performed.
In terms of maintenance of the regular planes, other factors that we need to consider is whether you need to enter in posteriorly to Gerota’s fascia to obtain an adequate margin and anteriorly to ensure the tumor can be mobilized safely off of the posterior wall of the stomach.
In light of these findings, on the cross sectional imaging which include MRI, our plan would be to perform a laparoscopic distal pancreatectomy. I think based on oncologic grounds, a spleen preserving procedure is probably reasonable. From looking at the scan, its likely technically possible although a vessel preserving procedure is likely not appropriate for this patient. Technical intraoperative factors will certainly influence that decision.
Dr. Moulton's imaging findings:
No formal tunnel dissection required
Normal ligation of splenic vein and splenic artery
Warshaw technique for splenic preservation
Tumor proximity to left adrenal gland
Hi my name is Carol-anne Moulton, I’m one of the surgeons here at TGH and an associate professor in the department of surgery. So I’ve had the ability to look at the MRI of this case that I’ve been asked to comment on. It has a mucinous or what appears to be a mucinous cystadenoma in the tail of the pancreas. To me, it looks like a pretty straightforward case. I agree with the decision to remove the tumor or cyst, give that it is unilocular and large and likely a mucinous cystadenoma. My preferred method of doing this particularly in a benign situation would be a laparoscopic distal pancreatectomy with or without the spleen.

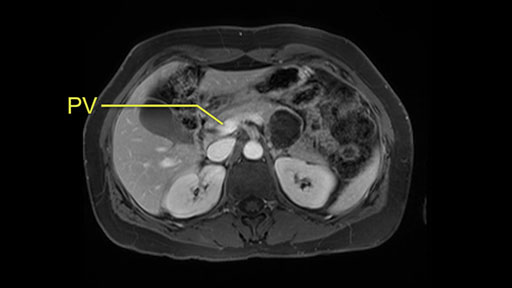
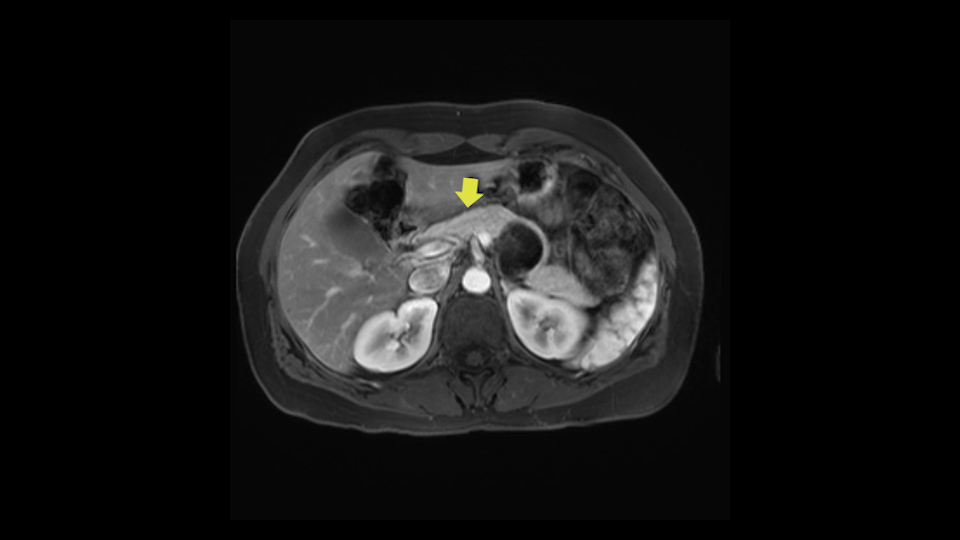
The slowing down moments or considerations that I give when I look at the scan and plan my distal pancreatectomy is how far away the tumor is to the portal vein and do I have to formally create a tunnel behind the pancreas on top of the portal vein or do I have to take the pancreas further to the left of the portal vein or the patient’s left of the portal vein. So here I can see that here is the tumor here. I can see that the tumor is a fair way away to the patient’s right and so I will likely not have to take or create the tunnel formally in this procedure. And that speaks a lot to the resection margins. So its important when you’re doing a distal pancreatectomy or any procedure potentially for oncologic reasons to get clearance of the tumor and to take the tumor kind of intact.
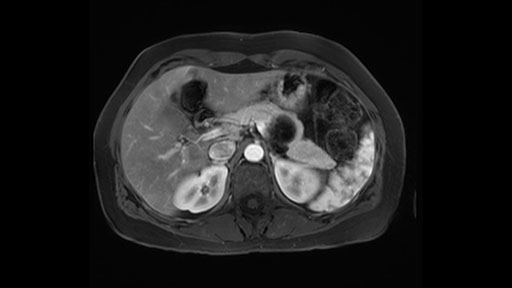
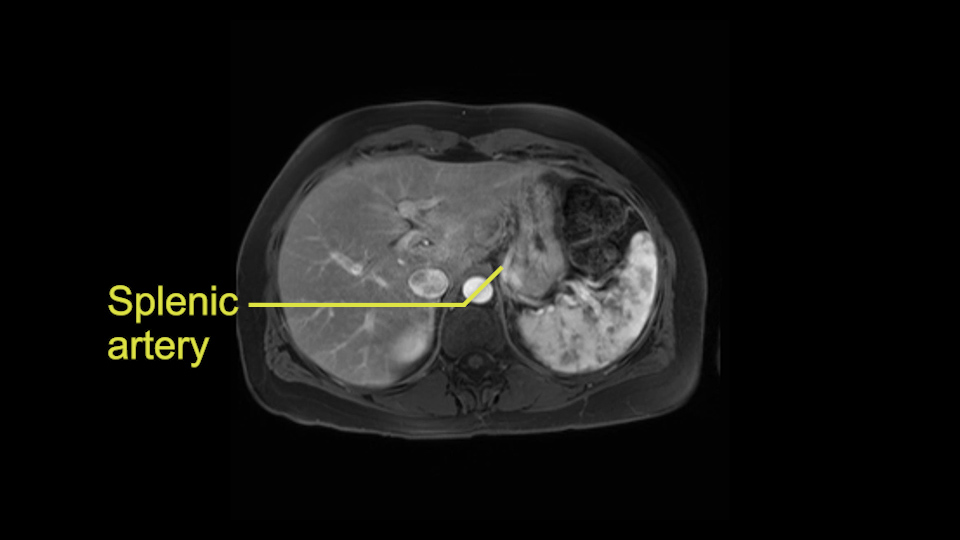
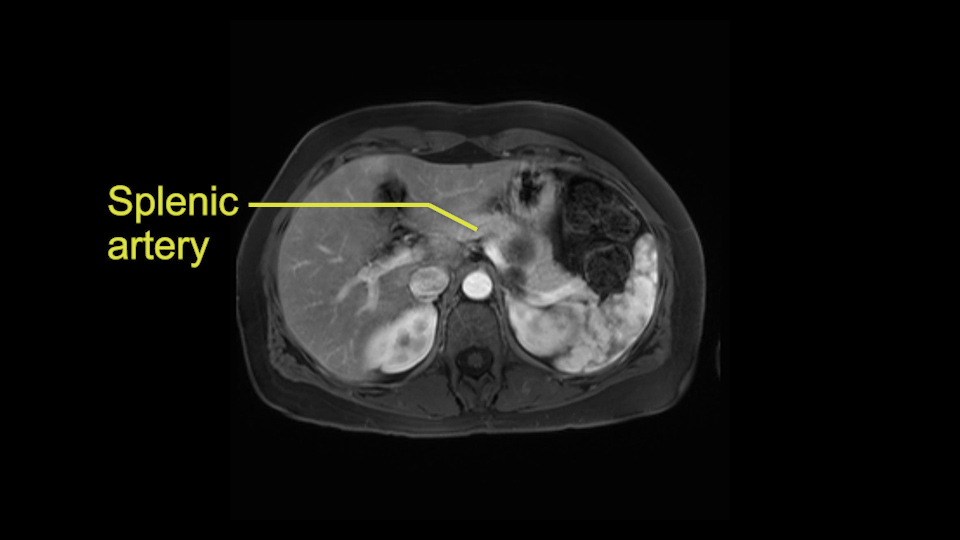
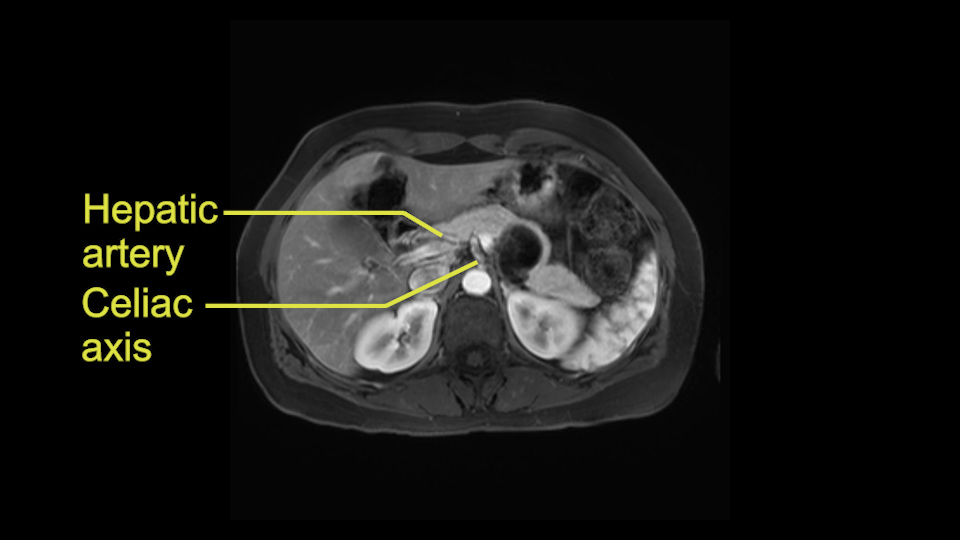
The second slowing down moment or consideration I give to a distal pancreatectomy is the anatomy of the portal vein and the splenic artery. And so I look here and the anatomy is pretty straightforward. The splenic vein comes off normally and runs behind the pancreas and I can see the artery superior to that, again coming off in a normal manner from the celiac axis. So those two things, the portal vein and the splenic artery will be taken normally in this procedure.

The third consideration in a distal pancreatectomy is whether I take the spleen or preserve it and I will try to always preserve it if I can. If it can be done safely and without too much difficulty or risk of bleeding. So the couple of considerations on the imaging that I look at is: Is the tail of the pancreas firmly embedded in the hilum of the spleen? I can see here that it isn’t and that it would likely be possible to preserve the spleen and I also look at the vessels and see whether the vessels are kind of firmly kind of intertwined in the distal part of the tail or whether we think we can actually separately take them with a stapler and remove all the tip of the tail of the spleen. So I think this would be a good candidate for a Warshaw technique, which is not preserving the splenic vein or artery but rather taking them as a segment and preserving the spleen. After this, the spleen would be getting all the blood supply from the short gastrics of the stomach. So that’s the third consideration in a distal pancreatectomy and the final thing is the retroperitoneum.

Sometimes with even benign lesions of the spleen you can have quite a lot of inflammation in the retroperitoneum and so I do think about and wonder whether I will have some difficulty in the retroperitoneum and I usually look at the scan for that purpose. It looks like there is no inflammation in the retroperitoneum. It does look very close to the patient’s left adrenal gland but knowing the planes and suspecting that there isn’t any active inflammation, this should be able to come off the left adrenal gland without any difficulty. But obviously prepared to take some of the left adrenal if that’s necessary in this procedure. So those are my procedure-specific slowing down moments in a distal pancreatectomy when I’m considering a laparoscopic approach. I think the patient-specific slowing down moments in this particular case I have discussed with the procedure-specific moments. I don’t really see any other issue or that I have to be careful of or consider.
Patient-specific findings:
Confirm no vascular involvement
Proximity of lesion to splenic vein, left adrenal gland, bowel loop
Preserve splenic vessels, spleen
Procedural slow-down moments:
Patient positioning
Port positioning
Mobilize splenic flexure
Expose splenic vein at inferior pancreas edge; careful handling of cyst
Splenic artery at superior pancreas edge
Transection margin at pancreas neck
Dissect pancreatic tail from splenic hilum
My name is Catherine Teh from the University of Santo Tomas and I am a HPB surgeon in Manila. I work in 3 different hospitals: Makati Medical Centre, St. Lukes Medical Centre and also in government at the National Kidney and Transplant Institute.
This patient has a pancreatic body lesion. Basing on the scan, I would recommend a spleen-preserving distal pancreatectomy - laparoscopic approach mainly because it appears that it is a benign lesion.
The preoperative MR is very very important; any scan for that matter. Whether it is a pancreatic protocol CT scan or the MR as presented, the diagnostic imaging plays a very big role. And with this we see that it’s a very well-defined cystic focus in the body of the pancreas. Although there are septal enhancements, very well demarcated, but there is no vascular involvement. However, the mass appears to be in contact with the splenic vessel, and the mass is also a little bit in touch with the left adrenal and also the loop of bowel. So looking at this, basing on the features, I think it’s probably a mucinous cystic lesion, it could possibly be a pseudocyst. But basing on the history, it appears like there is no history that would point out to a pseudocyst. And not an IPMN as well; I don’t see any side branches from the MRCP and the MR scan and although there is no axial T2 images available, and I truly find it easier to identify the septations on T2, and the hepatic cyst that is visible on this scan makes it hard to differentiate it from a simple or complex cyst which may be considered in a mucinous neoplasm with cystic or mucinous metastasis. Basically the contrast would help us in identifying the enhancing mural nodules or septations in the cysts. The MRCP is definitely helpful to identify if there is any side branch, if we are considering any IPMN.


So basing on this, it probably appears like this is a benign disease. We just need to make sure that we avoid the vascular structure of the splenic vessels. We try our best, meticulously, to preserve the splenic vessels, such to preserve the spleen and also to try to isolate it from the bowel loops that appears to be in contact and also spare the adrenal.

Although the value of the spleen-preserving distal pancreatectomy definitely is important, to avoid overwhelming sepsis. Although this is rare, but it could be very, very severe if it happens. Preoperatively, I would make sure that the patient would receive vaccination just in case any form of injury to the vascular structures would happen and that I would have to remove the spleen for that reason or any injury to the spleen as well, just in case.
So intraoperative decision making would probably change if there will be any massive bleeding encountered or unexpected findings that would change significantly if there is any vascular involvement.
I think the most important thing in doing the distal pancreatectomy in this case would be the positioning. I would position the patient in a way that would allow the maximum exposure with the minimal manipulation. So with that I normally would do a modified right lateral decubitus position with the right arm hyper-extended and perhaps the left arm just on an armrest and the left side would be raised about 60 degrees. And definitely make sure that the patient is plastered properly in the bed so that when we move the patient from side to side, then the patient wouldn’t fall. So this is because we would need to use gravity to expose the structures and avoid too much manipulation.
I think the port positioning is also an important aspect to be able to carry out this procedure. I would place a 12-mm port above the umbilicus just around the periumbilical area although I tend to go a little bit more towards the medial margin of the rectus abdominis so it’s a little bit towards the right and then just around it create like a semicircular and in an arc form putting in another 15-mm trocar at the left border of the rectus and then a 5-mm port at the anterior axillary line. Another 5-mm port probably can be placed at the epigastric area if it’s necessary. From the mid-clavicular line towards the anterior axillary line will be good to use as working ports.
So first step that we do: mobilize the splenic flexure first to visualize Gerota’s fascia and that would help bring down the colon and expose the pancreatic tail. So now that the pancreas is visible, division of the gastrocolic ligament will come into view. And a window can be created at the inferior edge of the pancreas to slowly lift the inferior edge to expose the splenic vein behind. This is the slow-down moment that I am talking about because the MR shows that there could be contact with the cyst. It’s important to know that to avoid perforation, to avoid rupture of the cyst, because we need to avoid touching the cyst, it is quite a size of 4.3 about 4cm.

So at this point, something that would be very helpful is to use gravity so that we can perhaps position the patient by moving the head down a little bit so that we can lift the pancreas and allow the stomach to retract superiorly, so we don’t have to retract the stomach with another instrument.
I think the splenic vein, once I have slowly teased it off from the cyst and from the retropancreatic parenchyma, I would put a vessel loop around it to serve as a traction. So once you have the vessel loop or probably umbilical tape, to retract or pull the pancreatic parenchyma while we slowly tease it off and try to move superiorly to be able to expose the splenic artery. That is again another slow-down moment because sometimes we think that it is the splenic artery at the superior edge of the pancreas, but it could also be the hepatic artery as it branches from the celiac artery.
So at this point it is important to choose the transection line once you have meticulously isolated the vessels and the pancreas, or the pancreatic body. Normally I would suggest to do the transection at the neck because this is the thinnest portion of the pancreas and the application of the stapler at the pancreatic parenchyma is, again, another slow down moment, not really a slow down moment but we should do it slowly. This is what we call as the peri-compression to try to compress the staple meticulously and gently into the neck, where we already have the entire dissection and mobilization of the pancreas. It is important to note that the compression should start slowly and not completely. So once you have opposed the jaw of the stapler, I’d wait a few seconds before I continue to press on and then another few seconds until I completely oppose the two jaws of the stapler. This usually will take about 2-3 minutes; you can relax, breathe, and let time do its job for you with the stapler.
It is important to think about what kind of stapler; the size of the staples that we use for the transection plane. Size diameter of the staples normally would be between 2.5mm and 3mm. If the pancreatic parenchyma is thicker than usual, I would use a 3mm which is usually the blue cartridge. If the neck area or the parenchyma is relatively thin, a vascular staple of 2.5mm would do its job.
I mentioned earlier that transection at the neck is the area that I would normally do as long as I have good margin from the lesion. And if the margin is not enough, I would go further to go to the right of the PV-SMV area at the junction and do the transection at that point.
Once the jaws have completely been opposed, then I would fire the staple and perhaps leave another few seconds before I unlock and release the staple so that would ensure opposing the pancreatic duct. Since this is a spleen preservation, we go from the medial to the lateral to try to remove as much of the tail as possible. We don’t want to leave the tail there at the hilum of the spleen. So again this is another slow down moment because the splenic vessels at the hilar area can still be injured while doing the dissection. So dissection just continues to remove the entire pancreas until the tail. This would complete the procedure.
Patient specific findings:
Proximity of lesion to PV-SMV
Distance from surrounding structures (left adrenal gland, bowel) and vessels
Locate IMV insertion to splenic/SMV
Procedure slowing down:
Trocar positioning
Inspection: check for peritoneal metastasis, small bowel
Be prepared for RAMPS, partial adrenal resection, as needed
Mobilize and hang pancreas
Identify, transect IMV if doing a splenectomy
Dissecting tunnel over SMV
Mobilize pancreas off HA, lymph node
Encircle splenic artery and vein
Use incision to extract specimen
Hello, my name is Marc Besselink. I'm a professor of HPB surgery at the Amsterdam UMC a Hospital of the University of Amsterdam. And today we'll be discussing a 40 year old woman who has a pancreatic cyst in the body of the pancreas. And I would like to talk to you about looking at the CT scan, deciding about the operation, type of surgery, and also some technical aspects.
So first, I'll show you the scan. Here's the traditional view, where you see the cyst, which is in the body of the pancreas. And you see over here, it's got a quite thick wall. And going a little bit back also, here you see a septation which is very important, because I think a septation is what separates this from, for instance, the pseudocyst of the pancreatitis. And also the location of the cyst you see here, abutting the adrenal gland and going down a bit more, it's also quite close to a bowel loop. So when thinking about this cyst: female, the location in the body of the pancreas, thick wall, septation, and as you can read in history, it was basically asymptomatic, so no signs of pancreatitis. So, this probably all points towards a mucinous cystic neoplasm.
Then the next thing to look at is the size. So until recently mucinous cysts would always undergo surgery. But with the recent new evidence based European guideline (2018)*, it’s a European guideline but it had all the world literatures involved, the cut-off for surgery is now actually four centimeter unless the cyst is smaller and patients have symptoms, for instance pain or pancreatitis, or whether there's a nodule. But for a asymptomatic mucinous cystic neoplasm, cut-off for surgery based on literature is now four centimeters. The risk of cancer in the cyst below four centimeters is lower than the risk of killing the patient by doing surgery. So I think that's a new addition to the guidelines and I think it's a very important one.
*[The European Study Group on Cystic Tumours of the Pancreas. Gut 2018;67:789–804. doi:10.1136/gutjnl-2018-316027]
So what type of operation are we going to do? It’s not a big cancer, it's a cyst. So I think this would be an ideal case for laparoscopic distal pancreatectomy. We could have a very long discussion about doing a splenectomy or not. For this case, in the European evidence based guideline, it is said that for mucinous cystic neoplasm, similar to resection for… for instance, main duct IPMN, you do an oncological resection, which means lymphadenectomy and splenectomy. So we'll speak about now about doing laparoscopic distal pancreatectomy with splenectomy.
Key features that I look at the imaging are: first I look at the distance between the cyst and the portal vein SMV confluence. So there are guidelines for this, they call the Yonsei guidelines, to decide to do it laparoscopically or open and basically it says that if it’s a cancer, at least a centimeter away from the celiac trunk or the venous confluence. This is a cyst. So maybe you could stretch that a bit, but you don't want to get into trouble there. So for this cyst if you look at it, it's nicely away from the confluence.
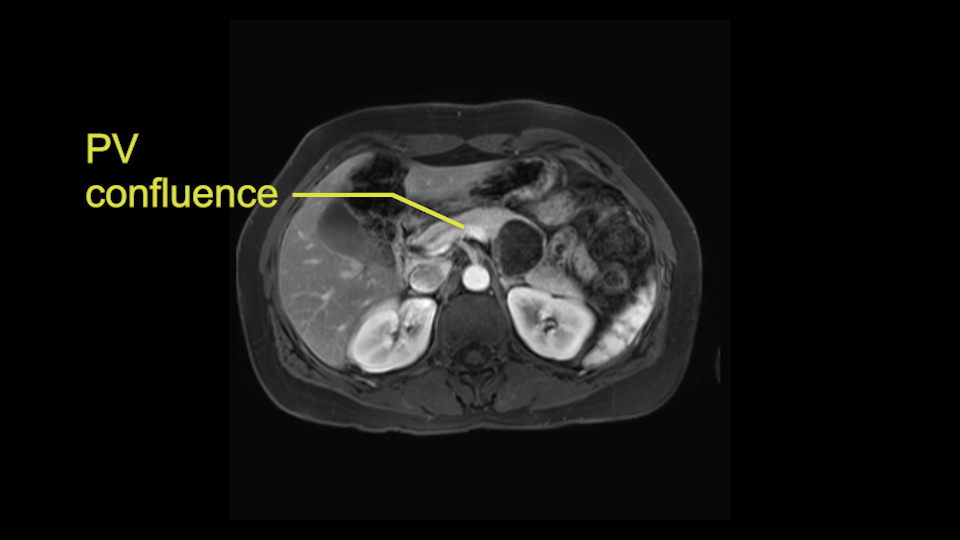
So unfortunately I cannot show you a coronal view but you can see it easily on this scan, going down first you see the celiac trunk and you see here, quite a nice distance between the celiac trunk and the beginning of the mucinous cyst. And if you go up here and follow down the portal vein confluence you also see a nice distance there.
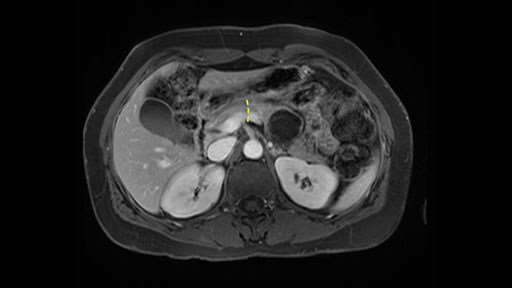
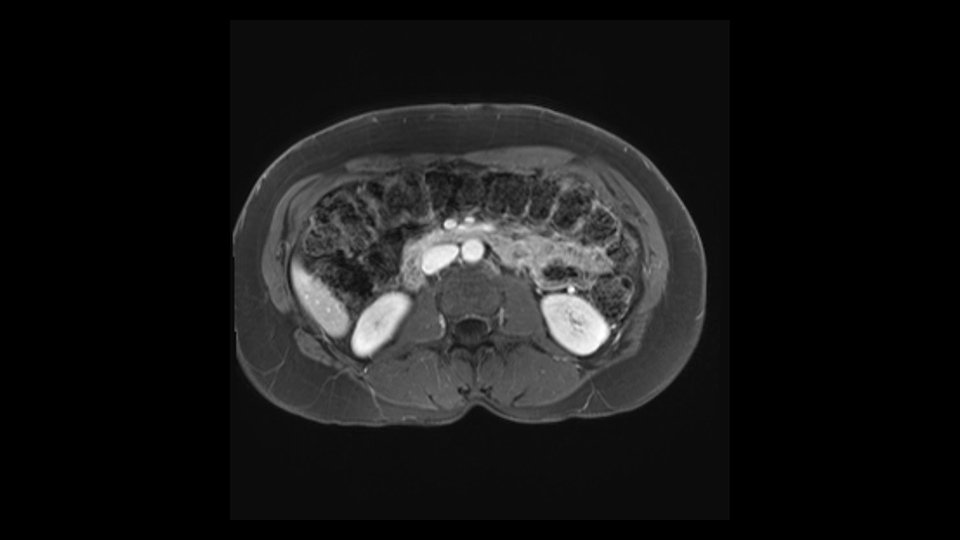
So what I would normally do in these patients, I would look at the abutment of any other organs, one, which is here, potentially the adrenal gland and two the small bowel. And two, look at the distance from the vessels which I would normally do in a coronal view. So you can easily measure the distance and third I look at the insertion of the inferior mesenteric vein. Now we can probably also see that on here. Although it's better on a CT scan and it's better on a coronal view, you want to know where the inferior mesenteric vein comes into either the splenic or the SMV, because that is typically a very important slow down moment when you mobilize the lower portion of the pancreas knowing where the inferior mesenteric vein comes in either the splenic vein or the SMV. So those are I think the three most important points for the CT scan.

So now we move on to the procedure specific moments. For a laparoscopic distal pancreatectomy, you have typical trocar positions which are in a C shaped form, where I think it's very important to always have a good distance between the trocars which is basically the width of a hand and obviously we have smaller hands and bigger hands but the width of a hand between the trocars. I typically would place three 12-mm trocars and one very, very high 5mm trocar and one very lateral 5-mm trocar.
You start with inspection. And in this case, I would have a look below the mesocolon to see if there's any small bowel involvement. If there is, it may be a good idea to start there and mobilize the loop a little bit. Free the peritoneum. Look for any metastasis; it is very unlikely but still I think it should be routinely done. Then during the operation, if you will encounter in fact that the small bowel is involved, which I do not suspect will be the case because this is a mucinous cyst and not a cancer. But if it is involved, you can in fact staple a sidewall, a single sidewall of the small bowel. Now the way to do that would be to loop the small bowel involvement, and place a stapler 90-degrees on the bowel. So by doing that, you would staple off one wall of the jejunum without narrowing it. So that is an easy trick.
After you've slung the pancreas, to the left of the cyst, and if you encounter any adrenal involvement later after you have transected the pancreas and you move to the left side of the patient towards the spleen, take either the entire or partial left adrenal gland with the resection. If you go underneath the adrenal gland, and it's probably best to do a full RAMPS (Radical Antegrade Modular Pancreatosplenectomy) procedure, that is where you take the Gerota’s fascia completely onto the mucinous cyst. And that's very crucial to get a radical resection if you think the adrenal gland is involved.
So at the beginning of the operation, after you’ve placed the trocars, mobilization of the pancreas, starting with the posterior mobilization of the entire pancreas. And then you can do it several ways. The way I personally prefer is to go underneath the pancreas. So you can sling it, you can hang it with a vessel loop. Now, there are two ways to do that. For a cancer, which this is not, but for a cancer, you would incise Gerota’s fascia and go underneath. So you would take Gerota’s fascia always with the specimen. You can have a debate on whether you should do that here as well. But I think strictly speaking, it's not necessary.
If you hang the pancreas then you move down towards the right side of the patient. You know your first slowing down moment is where the inferior mesenteric vein comes in the splenic vein or into the superior mesenteric vein, you have looked at that at the scan, so you know where to expect it. You can do two things in a procedure where you can preserve the splenic vein, you can preserve the IMV as well. But in this case where you want to do an oncologic resection with splenectomy, you will transect the inferior mesenteric vein.
Moving down to the right, you will encounter the superior mesenteric vein. Definitely a slowing down moment. And that's when you can start to make the beginning of a tunnel. You don't make the entire tunnel. Then you go to the cranial side of the pancreas. Also there you mobilize it fully. The slowing down moment is freeing the hepatic artery and the station 8 lymph node which is there which comes with a routine oncologic resection so you mobilize that off the hepatic artery and then you continue at the superior side of the pancreas, going up to the celiac trunk, taking also the lymph nodes on the left gastric artery and below the celiac trunk. After you've done that, you can complete the tunnel and also hang the pancreas there with a bit of vessel loop. So basically now you’ve got two vessel loops around the pancreas, you can hang the entire pancreas. From that comes, stapling of the pancreas. I typically do that first before transecting any vessels. You can staple the pancreas with various staplers. Depending on the size, if you cut it at the neck, which you should do for oncologic resection. You could probably take a thinner stapler than if you would go more to the left side of the pancreas. There's no conclusive evidence on which stapler to use.
You cut the pancreas and then it's time to go to the splenic vein and artery. I would advise to encircle them both. Again with vessel loops. You can take a quarter length vessel loop meaning take a full one and ask the nurse to cut it twice in halves; encircle the vessels, put the vessel loops around it and you can secure the vessel loop with a Hem-o-lok. Having done that, will make it easier for you to place the clips in exactly the right place. I would put Hem-o-lok clips, two on the patient's side, one on the specimen side; first going for the artery so there isn't any congestion and then going for the vein. After you’ve transected the splenic artery and vein, you move from the medial side to the lateral side, which is basically already for the most part mobilized in the beginning when you were slinging the pancreas on the left side.
So now is just taking the spleen with the specimen and you can extract the pancreas, the distal pancreas with the spleen. Very important point, my final point is where to extract. I know there are some people that enlarge a trocar site, I would definitely advise against doing that. There is for instance, a very recent, good, randomized trial in colorectal surgery, showing that if you enlarge the trocar side, the risk of hernia is about 10 to 15%. While as if you do a proper Pfannenstiel incision, meaning just suprapubic transverse skin incision and then -also important point -a transverse fascial incision. Many people then do a midline fascial incision which still gives you a higher risk of incisional hernia. If you do then a transverse skin, transverse fasciae the risk of incisional hernia is 0.5%. So, that's my final point for you. Thank you.
Acknowledgements
Thank you to the HPB Surgeons who contribute their time and expertise. This content is made possible through educational grants from:

![]()
Views and opinions expressed in all videos and module content are those of the individual surgeon and solely intended for surgical education purposes. We do not endorse any product, treatment or therapy.
Corporate Partners
If you are interested in becoming a Corporate Partner of the IHBPA please contact industry@ihpba.org
Find out more